As anticipated, Los Angeles County’s rising rate of COVID-19 spread caused it to be shifted Thursday from the federal government’s “low” virus level to “medium” — prompting calls from county officials to mask up indoors, get vaccinated and boosted and get tested at the first sign of illness.
According to federal and county data, the county’s cumulative seven-day rate of new COVID cases rose to 202 per 100,000 residents, up from about 176 per 100,000 last week. With the number topping 200, the county is now considered to have “medium” COVID levels, a designation that comes with recommendations for heightened precautions against virus spread.
The move will not trigger any immediate changes in health regulations in the county, which was already maintaining stepped-up precautionary recommendations that align with the CDC’s guidelines under the “medium” ranking — such as masking on public transit and high-risk settings such as hospitals and homeless shelters, widespread availability of vaccines and access to testing, including at-home tests.
The county still is not mandating indoor mask-wearing in all public settings, but it is being strongly recommended. Masks would become mandatory indoors if the county slips into the “high” COVID level. Reaching that mark would require a sharp increase in COVID-related hospitalizations.
Numbers of COVID-positive patients have been increasing in recent weeks, and the percentage of emergency room visits associated with the virus crept up to 5% over the past week — up from 4% the previous week. But so far, the overall statistics are still well within the CDC’s parameters for the “medium” COVID level.
Under CDC guidelines, counties in the “medium” category will move to “high” if the rate of new virus-related hospital admissions reaches 10 per 100,000 residents, or if 10% of the county’s staffed hospital beds are occupied by COVID-positive patients.
County Public Health Director Barbara Ferrer said the county’s current rate of new admissions is 3.4 per 100,000 residents, and the rate of hospital beds occupied by COVID-positive patients is just under 1.7%.
Ferrer said she remains “hopeful” that the county will avoid sliding into the “high” COVID community level, but only if residents and businesses don’t “shy away” from safety practices “that are known to reduce transmission,” such as indoor masking and ensuring people are up to date on vaccinations.
The recent increase in cases has been largely blamed on spread of the highly infectious BA.2 subvariant of the Omicron variant, which sparked a major surge in cases over the winter. But Ferrer on Thursday reported a dramatic increase in cases caused by the even more infectious BA.2.12.1 offshoot of the variant. According to the latest results, 27% of cases that underwent specialized testing to identify variants were found to be BA.2.12.1 — up from 3% a month ago.
The county has now also identified six cases of BA.4 and one case of BA.5, two variants that have caused widespread infections in South Africa.
Ferrer noted that the currently available COVID vaccines are still effective in preventing the variants from causing severe illness. She renewed her call for residents to get vaccinated and to get booster shots when eligible.
“The task in front of us is similar to the work we’ve had to do at other points over the past two and a half years — slowing transmission,” she said.
County Supervisor Holly Mitchell echoed Ferrer’s comments.
“We’ve got to continue to acknowledge the importance of masking while indoors … testing if exposed or testing if we intend to travel — before we travel and after we come back, testing if we feel ill or if we’ve been at a large gathering, and getting vaxxed and boosted,” Mitchell said.
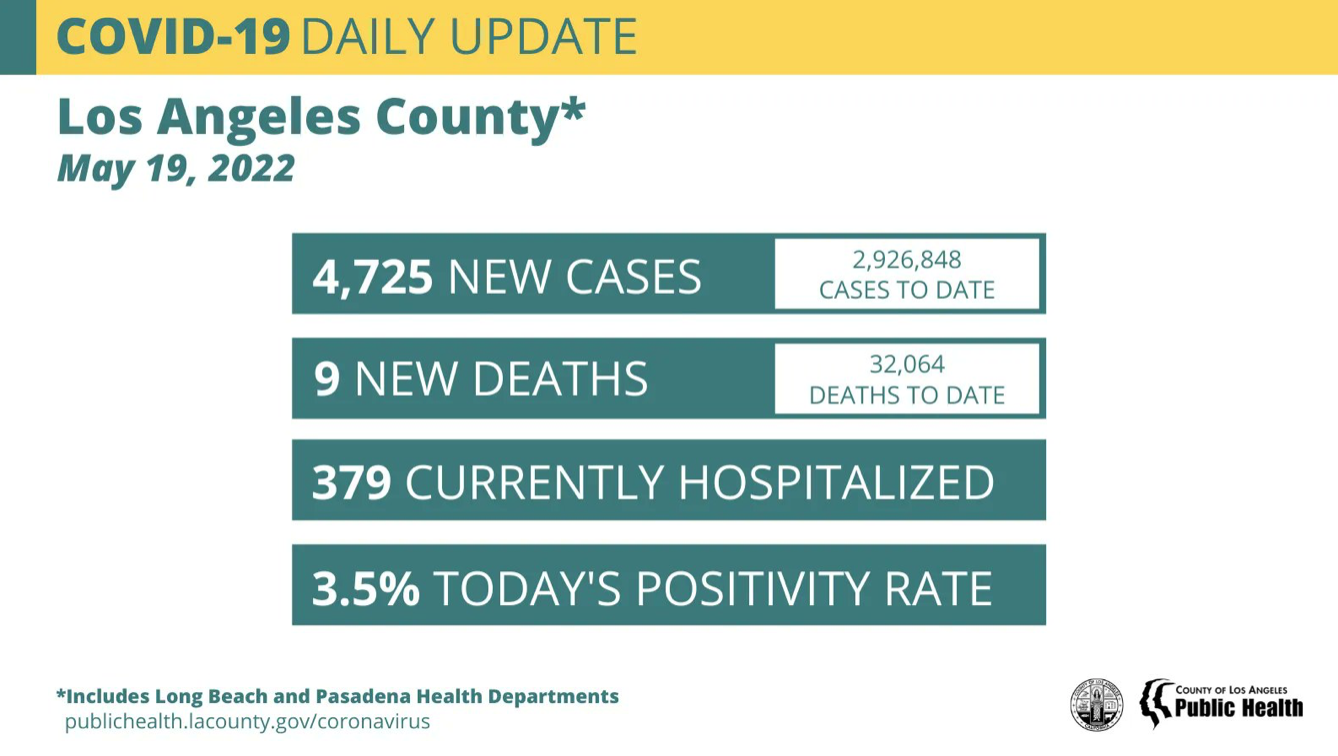
The county reported 4,725 new COVID infections on Thursday, lifting the overall total from throughout the pandemic to 2,926,848. Nine more virus-related deaths were also reported, raising the cumulative local death toll to 32,064.
As of Thursday, there were 379 COVID-positive patients in county hospitals, up from 363 on Wednesday. The number of those patients being treated in intensive care was 53, down from 55 a day earlier.
The average daily rate of people testing positive for the virus rose to 3.5%, up from 3.2% a day earlier.