View Winners →
View Winners → AHA reports significant increase in US cardiovascular deaths
More people died from cardiovascular-related causes in 2020, the first year of the COVID-19 pandemic, than in any year since 2003, with the largest increases in deaths among Asians, Blacks and Hispanics, according to the American Heart Association 2023 Statistical Update.
The association’s 2023 Statistical Update reported that the number of people dying from cardiovascular disease, or CVD, in the U.S. escalated during the first year of the pandemic from 874,613 CVD-related deaths in 2019 to 928,741 in 2020.
The rise in the number of CVD deaths in 2020 represents the largest single-year increase since 2015 and surpassed the previous high of 910,000 in 2003.
“While the total number of CVD-related deaths increased from 2019 to 2020, what may be even more telling is that our age-adjusted mortality rate increased for the first time in many years and by a fairly substantial 4.6%,” Dr. Connie W. Tsao, chair of the Statistical Update writing group, said in a statement.
“The age-adjusted mortality rate takes into consideration that the total population may have more older adults from one year to another, in which case you might expect higher rates of death among older people,” said Tsao, who is also a Harvard Medical School professor and cardiologist at Beth Israel Deaconess Medical Center in Boston. “So even though our total number of deaths have been slowly increasing over the past decade, we have seen a decline each year in our age-adjusted rates – until 2020. I think that is very indicative of what has been going on within our country – and the world – in light of people of all ages being impacted by the COVID-19 pandemic, especially before vaccines were available to slow the spread.”
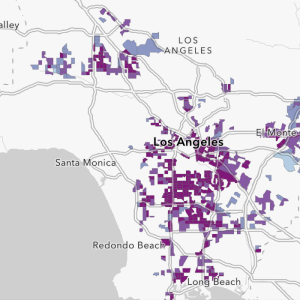
The largest increases in the number of cardiovascular-related deaths occurred among Asian, Black and Hispanic people — populations most impacted in the early days of the pandemic, according to the AHA.
“We know that COVID-19 took a tremendous toll, and preliminary data from the U.S. Centers for Disease Control and Prevention have shown that there was a substantial increase in the loss of lives from all causes since the start of the pandemic. That this likely translated to an increase in overall cardiovascular deaths, while disheartening, is not surprising. In fact, the Association predicted this trend, which is now official,” AHA President Dr. Michelle A. Albert said in a statement.
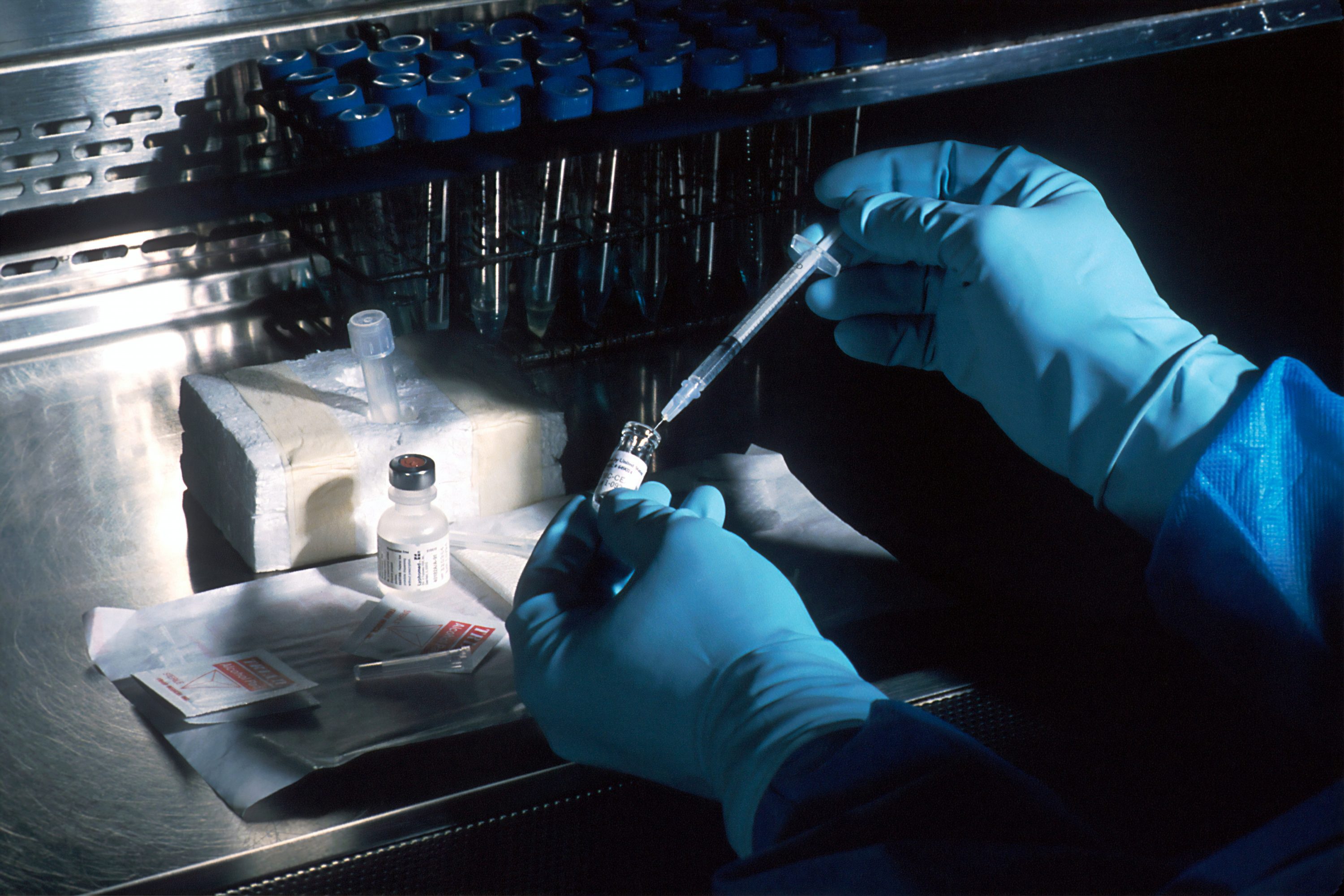
“COVID-19 has both direct and indirect impacts on cardiovascular health. As we learned, the virus is associated with new clotting and inflammation,” said Albert, the admissions dean and a professor at the UC San Francisco Medical School. “We also know that many people who had new or existing heart disease and stroke symptoms were reluctant to seek medical care, particularly in the early days of the pandemic. This resulted in people presenting with more advanced stages of cardiovascular conditions and needing more acute or urgent treatment for what may have been manageable chronic conditions. And, sadly, appears to have cost many their lives.”
According to Albert, who is the director of the CeNter for the StUdy of AdveRsiTy and CardiovascUlaR DiseasE, or NURTURE Center, at UCSF and a leader in health equity and adversity research, the larger increases in the number of coronary heart disease deaths among adults of Asian, Black and Hispanic populations appear to be linked with the people most often infected with COVID-19.
“People from communities of color were among those more highly impacted, especially early on, often due to a disproportionate burden of cardiovascular risk factors such as hypertension and obesity. Additionally, there are socioeconomic considerations, as well as the ongoing impact of structural racism on multiple factors including limiting the ability to access quality health care,” Albert said. “The American Heart Association responded quickly at the beginning of the pandemic to address the impact of COVID-19 and focus on equitable health for all. The Association launched the first-ever rapid response research grants calling on the research community to quickly turn around transformative science; established a COVID-19 CVD hospital registry through the Get With The Guidelines® quality initiative; and also made an unprecedented pledge to aggressively address social determinants while working to support and improve the equitable health of all communities. We are empowering real change that will save lives.”
Cardiovascular disease includes coronary heart disease, stroke, heart failure and hypertension/high blood pressure, according to the AHA. Coronary heart disease includes clogged arteries or atherosclerosis of the heart, which can result in a heart attack, and is the leading cause of death in the U.S.
Stroke continues to rank fifth among all causes of death behind heart disease, cancer, COVID-19 and unintentional injuries or accidents, the AHA reported. COVID-19 made the list of leading causes of death for the first time in 2020, the most recent year for which final statistics are available from the U.S. Centers for Disease Control and Prevention.
The 2023 AHA Statistical Update includes many references to COVID-19 and its impact on cardiovascular disease. Data points and scientific research findings are inserted throughout most chapters of the document, including those related to the risk factors for heart disease and stroke such as obesity, diabetes and high blood pressure, all of which also put people at increased risk for COVID. Many of the studies noted identify specific gender, race and ethnicity disparities.
Disparities don’t solely occur among age, sex and racial or ethnic groups, according to the Statistical Update’s writing committee. While the Update has been including a variety of social factors affecting health data in its report, the commentary noted that data from other underrepresented populations, such as LGBTQ people and people living in rural vs. urban areas of the U.S. are still lacking. The commentary authors note the lack of scientific research and cumulative data on the impacts of social identity and social determinants.
“We know that to address discrimination and disparities that impact health, we must better recognize and understand the unique experiences of individuals and populations. This year’s writing group made a concerted effort to gather information on specific social factors related to health risk and outcomes, including sexual orientation, gender identity, urbanization and socioeconomic position,” Tsao said. “However, the data are lacking because these communities are grossly underrepresented in clinical and epidemiological research. We are hopeful that this gap in literature will be filled in coming years as it will be critical to the American Heart Association’s goal to achieve cardiovascular health equity for all in the U.S. and globally.”
Globally, cardiovascular disease continues to be the no. 1 killer, taking the lives of more than 19 million people each year. However, the risk factors that lead to heart disease and stroke continue to disproportionately impact certain populations in the U.S. as well as around the world, according to the AHA.