By Peter Elkind
This story was originally published by ProPublica. ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Reporting Highlights
- Decades of Misbehavior: Lincare has repeatedly landed on Medicare’s equivalent of probation; the company has a dismal history of exploiting the government and ailing patients.
- Too Big to Ban: Despite Lincare’s track record, Medicare, which provides most of the company’s revenues, has never sought to bar the company from the Medicare system.
- Tolerating Wrongdoing: Faced with $60 billion a year in fraud, Medicare spends millions chasing companies but accepts penalties that are only a fraction of the profits made on misbehavior.
These highlights were written by the reporters and editors who worked on this story.
For Lincare, paying multimillion-dollar legal settlements is an integral part of doing business.
The company, the largest distributor of home oxygen equipment in the United States, admitted billing Medicare for ventilators it knew customers weren’t using (2024) and overcharging Medicare and thousands of elderly patients (2023). It settled allegations of violating a law against kickbacks (2018) and charging Medicare for patients who had died (2017). The company resolved lawsuits alleging a “nationwide scheme to pay physicians kickbacks to refer their patients to Lincare” (2006) and that it falsified claims that its customers needed oxygen (2001). (Lincare admitted wrongdoing in only the two most recent settlements.)
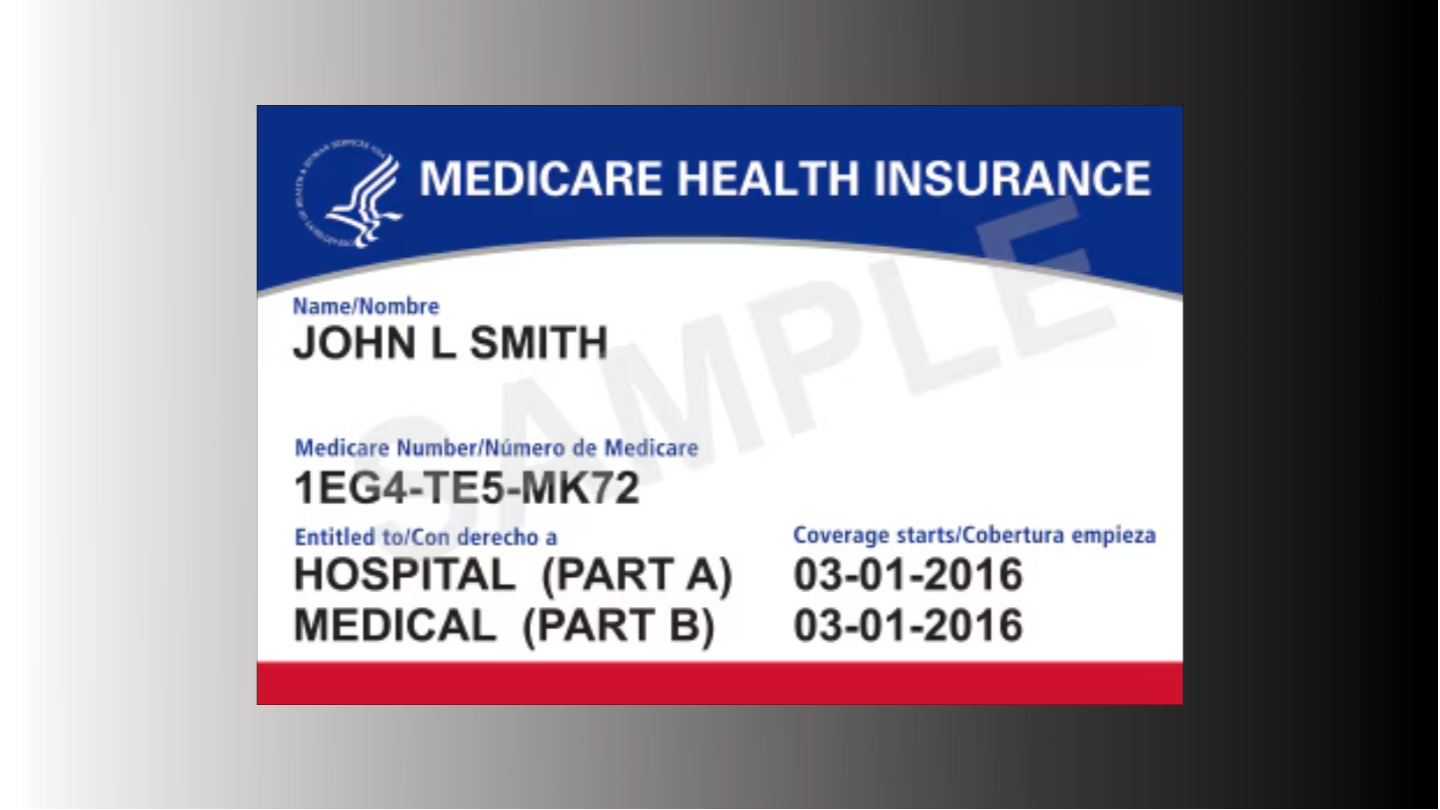
Such a litany of Medicare-related misconduct might be expected to provoke drastic action from the Department of Health and Human Services, which oversees the federal health insurance program that covers 1 in 6 Americans. Given that most of Lincare’s estimated $2.4 billion in annual revenues are paid by Medicare, HHS wields tremendous power over the company.
Sure enough, as part of the 2023 settlement, HHS placed Lincare on the agency’s equivalent of probation, a so-called corporate integrity agreement. The foreboding-sounding document includes a “death penalty” provision: Any “material breach” of the probation agreement, which runs for five years, “constitutes an independent basis for Lincare’s exclusion from participation in the Federal health care programs.” Such a ban could effectively kill Lincare’s business.
That sounds dire. Except that before that corporate integrity agreement was signed in 2023, Lincare was under the same form of probation, with the same death penalty provision, from 2018 to 2023, and violated its terms. From 2006 to 2011, Lincare was similarly on probation and also violated the terms, according to the government. And before that — well, you get the picture. Lincare has been on probation four times since 2001. And despite a pattern not only of fraud, but of breaking its probation agreements, Lincare has never been required to do more than pay settlements that amount to pennies relative to its profits.
This is not an aberration. While HHS routinely imposes the death penalty on small operations, it has never barred a national Medicare supplier like Lincare from continuing to do business with the government. Some companies, it seems, are too big to ban.
Lincare’s lengthy record of misbehavior isn’t a surprise to people in the medical equipment business. What is surprising is the federal government’s willingness to pull its punches with a company that has fleeced taxpayers and elderly customers again and again.
Federal officials have never pursued the company executives who oversee this behavior even though two of them, Chief Operating Officer Greg McCarthy and Chief Compliance Officer Jenna Pedersen, have worked at Lincare through all four of the company’s probationary periods. No one has faced criminal charges for activity the government’s own investigators deemed fraud.
Medicare has continued to pay Lincare billions even as many of the company’s customers revile it. Evaluations on customer-review websites are lacerating, and complaints to state attorneys general abound. On the Better Business Bureau’s website, 888 reviewers gave Lincare an average score of 1.3 out of 5. They cite dirty and broken equipment, charges that continue even after equipment has been returned, harassing sales and collection calls, and nightmarish customer service. As one person wrote in April, Lincare is “running a scam where they have guaranteed income” and “the customer can’t do a thing.”
HHS has always been reluctant to cut off big suppliers. Medicare’s first objective is to make sure nothing interrupts the flow of medications, devices and services to beneficiaries. And were HHS to seek to ban Lincare, the company would surely launch a long, costly legal war. But even if the cost of such combat reached many millions of dollars, it would still be a tiny fraction of the amount lost to fraud, which is yet another contributor to the soaring medical costs that bedevil the country. “This is taxpayer money,” said Jerry Martin, a former U.S. attorney who represented an ex-Lincare executive in a whistleblower suit against the company. “We need to pay people that don’t have four corporate-integrity agreements.”
Weak enforcement is not the only problem. Lincare is paid to rent oxygen equipment to patients, with HHS covering most of the monthly bills. But those rental fees often add up to many times what it would cost simply to buy the equipment. “If this were a rational country,” Bruce Vladeck, who ran Medicare from 1993 to 1997, told ProPublica, “the government would buy a million [oxygen] concentrators and pay Amazon or somebody to deliver them.”
In a seven-month investigation, ProPublica examined how Medicare’s largest provider of home medical equipment has managed to take advantage of its customers for a quarter of a century while fending off meaningful enforcement. ProPublica interviewed more than 60 current and former employees and executives, Medicare and Justice Department officials, patient advocates, and health care experts. ProPublica also reviewed dozens of court cases involving Lincare and thousands of pages of internal company documents, sales presentations and emails.
The investigation reveals a dismal picture of a company with a sales culture that depends on squeezing infirm and elderly patients and the government for every penny. Lincare employees are pressured to sell — whether a customer needs a product or not — on pain of losing their jobs.
And the company’s record of misbehavior and conflict extends far beyond its sales and billing practices. Lincare has paid $9.5 million in settlements for data breaches and mishandling patient and employee records. It has faced claims of violating wage rules, harassing customers with sales and collection calls, and tolerating racist comments to an African American employee. (Lincare lost the latter suit at trial and is appealing.) The company has repeatedly sparred in court with former executives, including a 2017 suit in which longtime executive Sharon Ford claimed that the company had cheated her out of a $1 million bonus. (A judge ruled in favor of Ford at trial before the case was overturned on appeal.) Ford testified that Lincare had earned an industry reputation as “The Evil Empire.” And when Lincare’s CEO, Crispin Teufel, resigned last year to become CEO of a rival company, Lincare sued him for breach of contract and misappropriating trade secrets. Teufel ultimately admitted to downloading confidential company records and was blocked from taking the new job. (Teufel did not respond to requests for comment. His replacement, Jeff Barnhard, took over as Lincare’s CEO in July 2023.)
Lincare declined multiple requests to make executives available for interviews. After ProPublica provided a lengthy document listing every assertion in this article, along with separate such letters to executives McCarthy and Pedersen, the company responded with a three-paragraph statement. It asserted that Lincare is “committed to delivering high-quality and clinically appropriate equipment, supplies, and services” but acknowledged “missteps in the past.” The company said its “new leadership” had “commenced a comprehensive review of our policies and procedures to help ensure we are complying fully with all state and federal regulations” and that “investments and enhancements we have made over the last several months will help prevent these issues from repeating in the future.” Lincare did not respond to follow-up questions requesting examples of the steps the company says it’s taking, including whether it has terminated any executives as part of this push.
When ProPublica asked a top Medicare enforcer why Lincare had eluded banishment, her answer suggested she views probation as a continuing ed class rather than a harsh punishment. “It’s like taking a college course,” said Tamara Forys, who is in charge of administrative and civil remedies for HHS’ Office of Inspector General. “At the end of the day, it’s really up to you to change your corporate culture and to study, to learn to pass the class … to embrace that and take those lessons learned and move them forward.” A spokesperson for the Centers for Medicare and Medicaid Services, which runs Medicare, declined to comment on Lincare but said the agency “is committed to preventing fraud and protecting people with Medicare from falling victim to fraud.”
There’s little incentive to refrain from misbehaving in an environment that tolerates bad behavior, said Lewis Morris, who was chief counsel to HHS’ Office of Inspector General from 2002 to 2012. “As long as that [settlement] check is less than the amount you stole, it’s a good business proposition.”
Indeed, Lincare has counted on the government’s tepid response, two former company executives told ProPublica. Top management, they said, responds to fraud warnings by conducting a cost-benefit analysis. “I’ve sat in meetings where they said, ‘We might have $5 to $10 million risk — if caught,’” said Owen Kirk Staggs, who ran one of Lincare’s businesses in 2017 and fell out with the company. “‘But we’ve made $50 million. So let’s go for it. The risk is worth the reward.’”
Libby, Montana, provides a glimpse of the way Lincare operates. Oxygen is an urgent need in this mountain town of 2,857. Libby suffers from the lingering effects of “the worst case of industrial poisoning of a whole community in American history,” in the words of the Environmental Protection Agency. An open-pit vermiculite mine, which operated from 1963 to 1990, coated the area — and residents’ lungs — with needle-like asbestos fibers. More than 2,000 Libby citizens have been diagnosed with respiratory diseases since then; some 700 have died.
Hundreds of ailing residents relied on Lincare for home concentrators, which provide nearly pure oxygen extracted from room air. Medicare and Medicare Advantage plans (which the government also funds) covered 80% of the monthly rental of about $135; patients paid the remaining 20%.
In 2020, Brandon Haugen noticed something suspicious in Lincare’s bills. Haugen was a customer service representative at the company’s local distribution site, one of 700 such locations around the country. (Lincare serves 1.8 million respiratory patients in 48 states.)
Lincare was allowed to charge patients and their insurers for a maximum of 36 months under federal rules. After that point, patients could use the equipment without further charge. Lincare, however, kept billing local patients and their Medicare Advantage plans far beyond 36 months — in some cases, for years. To Haugen, this looked like fraud.
Haugen conferred with center manager Ben Montgomery. The two, who had grown up in the area, had been buddies since seventh grade, after getting to know each other at summer Bible camp. Then 38, earnest and just beginning to gray out of their boyishness, the two men were concerned. The patients the men dealt with were their neighbors.
A regional Lincare manager assured them that charging beyond 36 months for Medicare Advantage patients “is the correct way to bill.” Skeptical, Montgomery raised the issue with Lincare’s headquarters in Clearwater, Florida. Lincare’s compliance director told him, according to Montgomery, that “it’s the patients’ problem to fix it if they want it to stop”; that was “just how it worked.” Further questions, sent to Lincare’s chief compliance officer, Pedersen, went nowhere. “It seemed pretty obvious they were well aware of this,” Montgomery told ProPublica. “For me, these were my customers that you were screwing over.”
Among them was Neil Bauer, now 80, who lives in a ramshackle house “out in the boondocks,” as he put it, 38 miles southeast of Libby. Bauer spent his career as a barber, head of investigations for the county sheriff’s department and a member of the local school board. He’s been on oxygen for more than a decade and quickly gets short of breath. “I can’t do stuff so much now,” he said. His wife is on oxygen, too. “We just have a sick family,” Bauer said.
Lincare had kept billing Bauer for his concentrator for seven years after it was supposed to stop. The monthly copays weren’t huge, but they added up to $2,325 that he shouldn’t have been charged over that period, a daunting sum for Bauer, who lives on a fixed income — and a hefty mark-up over the cost of the equipment, which can be purchased online for $799. For its part, Medicare Advantage paid Lincare $9,299 for Bauer’s concentrator during this period, along with another $5,760 for the months Lincare was legally permitted to bill. All told, the rental payments to Lincare, during authorized and unauthorized periods, were $16,547 for that one $799 piece of equipment. “We paid forever,” said Bauer. “Never was I told that we could have one without having to pay anything.”
Haugen and Montgomery studied billing records. Among the customers in their tiny office, Lincare was improperly charging at least 33 people and their Medicare plans. The two began to wonder how far this problem extended. An employee in Idaho confirmed the same practice was occurring there. “In my mind,” Montgomery said, “I went, ‘This is Libby, Montana. Multiply that by every center in the country. This is obviously a lot bigger deal.’”
Montgomery and Haugen had seen enough. On Jan. 18, 2021, they emailed a joint resignation letter to Lincare’s top management, recounting their concerns about billing that “likely affects thousands of patients company wide.” Citing the lack of response from corporate officials, they wrote, “we can only conclude that this is a known issue that is being covered up by Lincare.”
Haugen had 10 children. Montgomery had four. Neither man had another job lined up. “Had this not happened,” said Montgomery, who had been at the company for 13 years, “I would have seen myself retiring from Lincare.”
Instead, they became whistleblowers. They retained a law firm and sued Lincare in Spokane, Washington, the site of Lincare’s regional headquarters. After federal prosecutors decided to back the case, Lincare settled in August 2023. The company admitted to overbilling Medicare plans and patients across the country for years and paid $29 million to settle the matter, with $5.7 million of that going to Montgomery, Haugen and their lawyers. Dan Fruchter, the assistant U.S. attorney leading the government’s case, told ProPublica that the overbillings likely involved “tens of thousands” of patients.
Lincare agreed to its fourth stint of probation with HHS; the new corporate-integrity agreement took effect on the day after the previous one expired. The conduct Montgomery and Haugen flagged had gone on for years while the company was already on probation. But Lincare got the government lawyers to agree that nobody would try to impose the Medicare death penalty. Lincare asserted in the settlement that it had installed software (which it did only after learning of the government investigation) that will prevent billing beyond 36 months. Lincare promised to ensure “full and timely” compliance with the agreement and prevent future wrongdoing.
Medicare fraud, including in the “durable medical equipment” category that Lincare operates in, has long been an intractable problem. It cost the U.S. Treasury an estimated $60 billion in 2023 alone.
The government deploys large sums to try to stop it. HHS’ inspector general’s office has a $432 million budget and a staff of 1,600. Those resources are effectively extended by whistleblowers — most of the cases against Lincare have been such suits — who can receive a percentage of a civil settlement if they reveal wrongdoing, and by federal prosecutors, who can also bring cases or join those filed by whistleblowers. Last year HHS recovered $3.2 billion from fraudulent schemes.
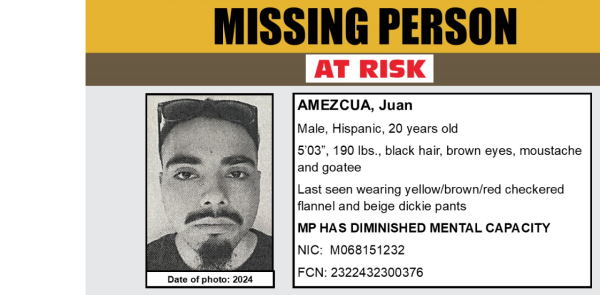
But the agency’s enforcers have wielded their biggest deterrent almost entirely against small perpetrators. In 2023, they banned 2,112 small firms and individuals from Medicare reimbursement.
HHS hasn’t done the same with companies that operate on a national scale. Forys, the agency enforcer, said she worries that expelling a big provider from Medicare could leave customers in the lurch. In April, Inspector General Christi Grimm defended her office’s work in congressional testimony but also asserted that its resources are inadequate. A lack of staff keeps it from even investigating “between 300 and 400 viable criminal and civil health care cases” annually, she testified, as well as more than half the fraud referrals from Medicare’s outside audit contractors.
A different reason for going easy on big companies was suggested by Vladeck, the former Medicare chief. Seeking to bar a large supplier for repeatedly violating probation would require exhaustive documentation and years of litigation against squadrons of well-paid corporate lawyers. As a result, Vladeck said, “there’s a real incentive, from a bureaucratic point of view, to just slap their wrist, give them a kick and make them apologize. … It’s a cost of doing business.”
There are steps enforcers could take, but almost never do, that would make companies take notice, according to Jacob Elberg, a former federal prosecutor who is now a professor at Seton Hall Law School. (Among his publications is a 2021 law review article titled “Health Care Fraud Means Never Having to Say You’re Sorry.”) Elberg’s research shows that HHS and prosecutors tend to negotiate far smaller civil settlements than the law allows, and they rarely prosecute company executives. They also almost never take cases to trial. In short, enforcers have long signaled to companies that they’re looking for a smooth path to a cash payment rather than a stern punishment for a company and its leaders. “It is generally a safe assumption,” Elberg said, “that the result will be a civil settlement at an amount that is tolerable.”
For its part, Congress may soon be weighing a new law that would reshape how the oxygen industry is paid by Medicare. But rather than clamp down on corporations, the legislation seems poised to do the opposite. A new bill called the SOAR (Supplemental Oxygen Access Reform) Act would hand companies like Lincare hundreds of millions more, by raising reimbursement rates and eliminating competitive bidding among equipment providers. Advocates say the legislation will help patients by making some forms of oxygen more available and improving service. But along the way it will reward Lincare and its rivals.
Congress has a history of treating oxygen companies generously. For years, lawmakers set Medicare reimbursements for oxygen equipment at levels that even HHS, in 1997, characterized as “grossly excessive.” Over the succeeding decade and a half, Lincare took advantage, snatching up hundreds of small suppliers and becoming the industry’s largest player.
In 2006, under pressure to reduce costs, Congress approved steps to curb oxygen payments, including the introduction of competitive bidding and the 36-month cap on payments for equipment rentals. But even those strictures were watered down after the industry poured money into political contributions and lobbyists, who warned that cuts would harm elderly patients.
Lincare compensated by amping up strategies that generated profits, with little apparent regard for Medicare’s rules, which say it will reimburse costs for equipment only when there is evidence of “medical necessity.” The company aggressively courted doctors and incentivized sales, through bonuses the company paid for each new device “setup.” According to a 2016 commission schedule, reps could earn $40 for winning an order for a new sleep apnea machine, $100 for a new oxygen patient and $200 for a noninvasive ventilator. The entire staff of each Lincare center could receive a small bonus for signing up a high percentage of new patients for automatic monthly billing. Patients who refused auto-billing, a company document advised, should be warned they might face “collection activity” and service cutoffs. “Sales is our top priority!” declared a 2020 PowerPoint to train new hires.
Once it had a customer, Lincare would pitch them more costly products and services. One way Lincare did this was through a program called CareChecks. Promoted as a “patient monitoring” benefit, CareChecks were aimed, according to a company presentation, at generating “internal growth.” If a patient exhibited a persistent phlegmy cough, Lincare could persuade their doctor to prescribe a special vibrating vest to loosen chest mucus. Nebulizer patients might be candidates for home oxygen. Patients using apnea devices were potential candidates for ventilators. “We’d make patients think we were coming in clinically to assess them,” a former Lincare manager said, “when really it was to make money off of them.”
Selling replacement parts could also be lucrative. At Lincare call centers that sold items like hoses, masks and filters for CPAP machines (used to treat apnea), hundreds of commissioned agents in Nashville, Tennessee, and Tampa, Florida, were equipped with programs displaying what items each patient was eligible for under Medicare. By law, patients had to request replacement parts. But frequently, that wasn’t what happened, according to Staggs, who oversaw the CPAP business in 2017. He discovered that top salespeople, whose bonuses could total $8,000 a month, averaged just a few minutes on the phone per order. That wasn’t nearly enough time to identify what items, if any, customers actually needed. Staggs listened to recorded calls and found that, after reaching customers, agents often placed them on hold until they hung up, then ordered them every product that Medicare would cover.
At Lincare, results were closely tracked and widely shared in weekly emails displaying the best and worst performers in each region. Notes taken by one manager show supervisors’ performance demands during weekly conference calls: “Unacceptable to miss goal … stop the excuses … If this is not being done, wrong [center manager] in place … If you’re not getting O2 and not getting Care Checks — you shit the bed. Stop accepting mediocre, lazy responses ….”
“If we didn’t meet our quota, they were going to chop our heads,” said former Illinois sales rep Sandra Gauch, who worked for Lincare for 17 years before joining a whistleblower suit and quitting in 2022.
One salesperson was so fearful of missing her quota, according to Gauch, that she signed her mother up for a ventilator that she didn’t need. A company audit in 2018 found that only 10 of 56 ventilator patients at one center were using them consistently. Some patients hadn’t used their devices for years. Yet Lincare kept billing Medicare.
Only one thing mattered as much as maximizing new equipment rentals, according to former employees and company documents: minimizing customers’ attempts to end rentals. A call to retrieve breathing equipment meant that it was no longer wanted or being used, and Lincare was supposed to retrieve it and promptly stop billing Medicare and the patient. The person’s health might have improved. They might have gone into the hospital — or died. The reason didn’t matter; at Lincare, “pickups” were a black mark, deducted from employees’ performance scores, jeopardizing their bonuses and jobs.
As a result, employees said, such requests were dreaded, delayed and deterred. Clinical staff were sent to “reeducate” customers to keep using their devices. Patients were told they’d need to sign a form stating they were acting “against medical advice.”
Lincare managers made it clear that pickups should be discouraged. In a 2010 email, an Ohio center manager instructed subordinates: “As we have already discussed, absolutely no pick-ups/inactivation’s are to be do[ne] until I give you the green light. Even if they are deceased.” In 2018, an Illinois supervisor emailed her deputies that pickups were barred without her explicit approval: “Not even Death that I don’t approve first.”
In February 2022, Justin Linafelter, an area manager in Denver, responded to the latest corporate email celebrating monthly “Achievement Rankings” for oxygen sales by pointing out that almost all of the centers atop the rankings had at least 150 “pending pickups,” customers who weren’t using their equipment but whom the company appeared to still be billing. “Some of these centers are just ignoring pickups to make this list.”
That was only one of Linafelter’s concerns. In July of that year, he emailed headquarters, saying he no longer had “the resources to be successful at my job.” The customer service staff in Denver had been cut in half, Linafelter explained, and he’d been barred from hiring replacements. Denver’s remaining staff was “at a point of exhaustion,” threatening patient care.
The morning after Linafelter expressed concerns to Lincare in 2022, he was summoned to a conference call with the head of HR and fired, for what he was told was a “corporate restructuring.” Linafelter, who had worked at Lincare for nine years, said, “I got thrown away like a piece of trash.”
Other former employees offer similar accounts. In 2020, Jillian Watkins, a center manager in Huntington, West Virginia, repeatedly alerted supervisors that Lincare was improperly billing for equipment that patients weren’t using. Lincare blocked her from firing a subordinate who’d falsified documents supporting the charges, then fired Watkins, citing “inadequate direction and leadership.”
Then came a series of turns. Pedersen, the chief compliance officer, effectively confirmed Watkins’ assertions, belatedly alerting the government about $486,000 in improper billings by Lincare. But Pedersen blamed the billings on Watkins, writing to Medicare that the company had “terminated” her to “prevent [the problem] from recurring.” After Watkins sued, Pedersen admitted in a deposition that Watkins’ firing “had nothing to do with the overpayment.” In April 2024, a federal judge ruled that Watkins had presented “a prima facie case of retaliation.” The suit was privately settled in mediation.
Staggs, too, was ousted, he said, after he warned top Lincare executives about improper practices at the CPAP call centers. Staggs emailed a Lincare HR officer: “Patients are being shipped supplies that they never have ordered. … This is fraud and I have gotten zero support or attention to this matter when I raise the issue to my leadership.” Only months after starting, he was fired in November 2017. He later filed a whistleblower suit; Lincare denied wrongdoing. After the U.S. attorney’s office in Nashville declined to join the case in 2022, Staggs withdrew the action.
Staggs’ account of improper billings matches an industry pattern that appears to continue to this day. In a 2018 report, HHS’ inspector general estimated that Medicare had paid more than $631 million in improper claims for CPAP and other supplies over a two-year period. Another HHS analysis identified an additional $566 million in potential overpayments for apnea devices.
The agency’s oversight “was not sufficient to ensure that suppliers complied with Medicare requirements,” the 2018 report concluded. Six years later, HHS has not taken public action against Lincare relating to CPAPs.
Today, fraudulent billing among Medicare equipment providers remains a “major concern,” according to the inspector general. The agency says it continues to review the issue.
Doris Burke contributed research.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox. Republished with Creative Commons License (CC BY-NC-ND 3.0).