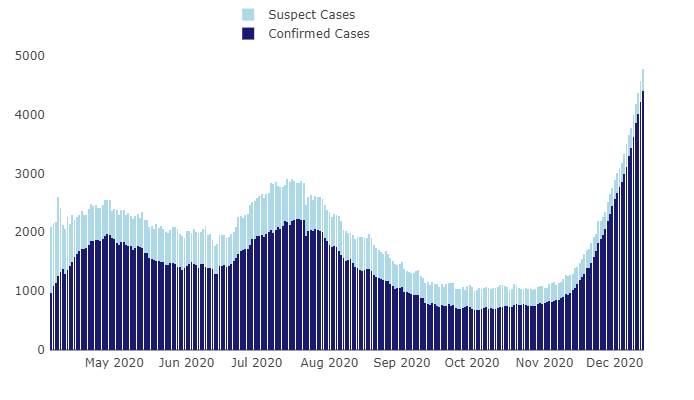
The number of hospitalizations due to confirmed and suspected COVID-19 cases in California reached a total of 14,578 Monday, an increase of 618 from the previous day. The number of ICU patients due to confirmed and suspected COVID-19 cases in the state reached a total of 3,078, an increase of 141 from the day before.
In Southern California — a region comprised of Los Angeles County, Orange County, Riverside County, San Bernardino County, San Luis Obispo County, Santa Barbara County, Ventura County, Inyo County, San Diego County, and Imperial County — ICU availability plummeted to 1.7% Tuesday morning.
As of Monday, ICU capacity was at 0% in Orange and Riverside counties. “San Bernardino County also had 0% of its capacity remaining Monday under the state’s official designation — which doesn’t include available intensive care beds for infants and children and is tweaked if a disproportionate number of beds are being used for COVID-19 patients — spokesman David Wert said,” according to reporting from The Press-Enterprise. In Los Angeles County, only 56 adult ICU beds remained Monday, Dr. Christina Ghaly, director of the Department of Health Services, said during a press briefing.
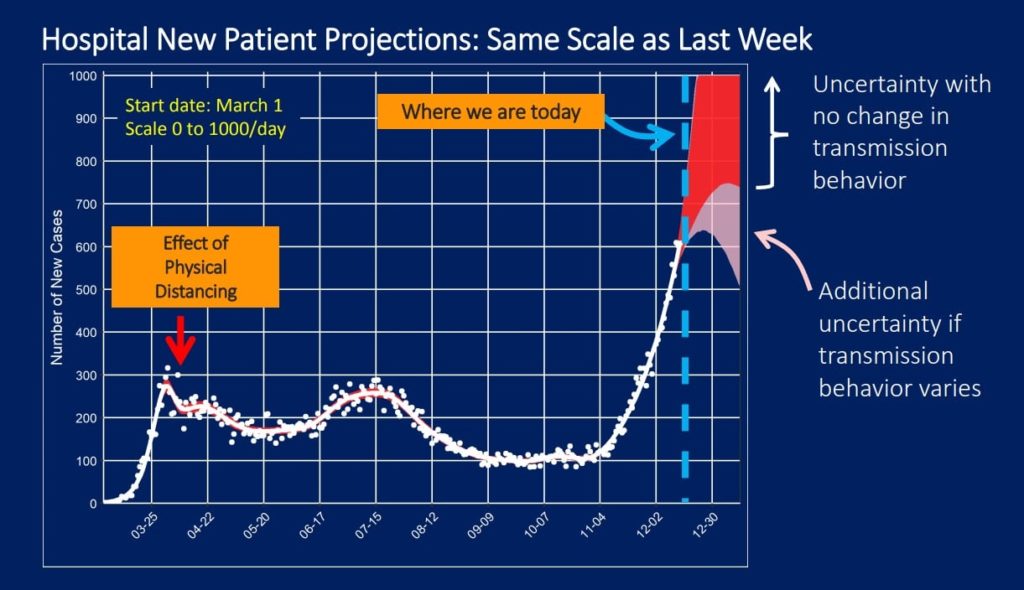
The shortages come as L.A. County experiences a wave of COVID-19 hospitalizations.
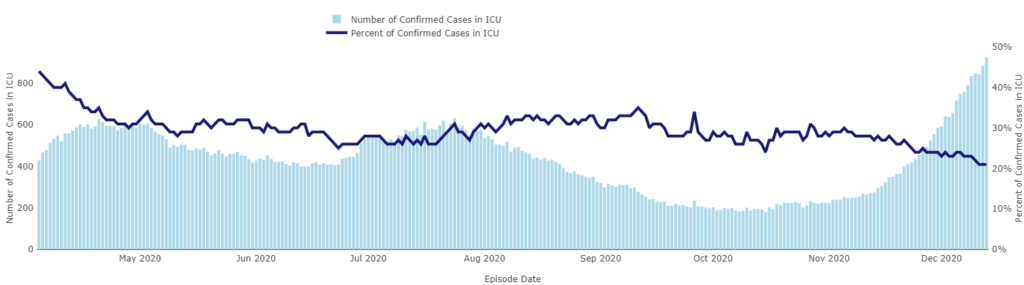
In L.A. County, there are 4,203 people with COVID-19 currently hospitalized and 21% of these people are in the ICU, an increase of more than 1,200 patients from Dec. 7 when the daily number of people hospitalized with the virus was 2,988. Since Dec. 1, the county has surpassed previous all-time highs every day.
Monday, Public Health confirmed 48 new deaths and 7,344 new cases of COVID-19, reflecting a reporting lag from one large lab; this lab started reporting the backlog of cases Monday.
Since the beginning of the surge on Nov. 1, cases have increased 625% with younger people continuing to drive the increase in community transmission in the county. More than 70% of cases are from people under the age of 50 years old.
However, the steepest increase in hospitalizations is experienced by older residents. Residents 80 and older have consistently experienced the highest rates of hospitalization among all age groups in L.A. County followed by residents 65 to 79 years old, and residents 50 to 64 years old.
Almost half of the county’s ICU beds are occupied by COVID-19 patients. By next weekend, there are likely to be over 5,000 patients hospitalized and more than 50% of ICU beds occupied by COVID-19 patients.
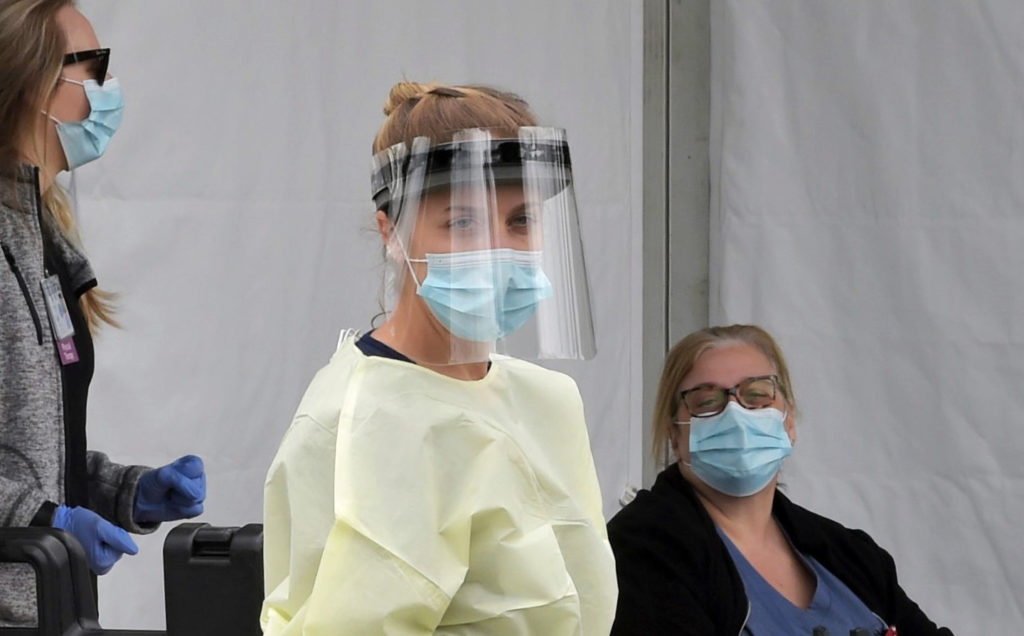
ICU staffing is just as much of a concern as the number of available beds. Every bed needs to be staffed by highly trained and skilled healthcare workers. The recent surge in cases has resulted in huge increases in cases among healthcare workers. In the last two weeks there have been over 3,400 new cases among healthcare workers. In early November there were 40 new cases among healthcare workers per day; last week there were nearly 250 cases among healthcare workers per day.
“Many folks may be thinking that this is just not anything to be really worried about because hospitals can just add more beds. The reality is every bed needs to be staffed by highly trained and skilled healthcare workers, and we don’t have an endless supply of healthcare workers, and those that are here saving lives every day are exhausted,” said Dr. Barbara Ferrer, director of Public Health.
The county has already added 13% more ICU beds as compared to the summer but Ghaly said, “That durability is not infinite. We cannot maintain this rate of increase. We will physically exhaust ourselves.”
She noted that some hospitals have already begun to limit non-essential procedures.
“We need to brace ourselves that this [hospital] case volume has not yet reached a peak and will keep growing.”
Officials hope to see the effects of the regional stay-at-home order by around Christmas but whether that data reflects good or bad news depends on how closely individuals are adhering to guidance.
The first COVID-19 vaccine was administered in Los Angeles County Monday. The first shipment arrived at one of nine sites, with the remaining eight sites receiving their shipment Tuesday and Wednesday. The current expected initial allocation for L.A. County is 82,875 doses, two additional allocations are expected in December. This does not include allocations for the cities of Long Beach and Pasadena, which have their own independent health departments and are receiving their own allocations.
“Because it is likely to take a few months to have enough vaccine available to immunize the millions of individuals who live and work in L.A. County, in the meantime, we all must continue to remain extremely diligent in reducing transmission of the virus,” cautioned Ferrer. “We continue to see extremely high numbers of new cases, hospitalizations and deaths from COVID-19 — the surge we are experiencing is alarming. If you are not playing by the rules, to be blunt, you are part of the problem, and at this point, you are contributing to these distressing increases in cases, hospitalizations, and deaths.”
The nine sites have been working with the Los Angeles County Department of Public Health and EMS to make arrangements to redistribute vaccine so that every acute care hospital that serves COVID-19 patients receives a pro-rata share of this initial allocation.
A second allocation of the vaccine that should arrive later this month will allow for a distribution of vaccines to all health care personnel and residents at skilled nursing facilities in the county, along with continued distribution to frontline healthcare and EMS personnel.