Huntington Medical Research Institutes senior scientist’s work considered a game-changer

We’ve all heard the phrase “better together” throughout the pandemic over and over again; however, that is exactly what Dr. Anju Vasudevan, Huntington Medical Research Institutes’ (HMRI) senior research scientist and scientific director for the angiogenesis and brain development research program, has found to be true in her recently published co-authored study on brain cell therapy for psychiatric and neurological disorders ranging from autism and schizophrenia to epilepsy and severe depression.
Vasudevan and her colleagues’ work published on July 13 in Molecular Psychiatry is considered to be a game-changing breakthrough uncovering why cell-based therapies are failing, and providing a missing link in the process, that when the right vascular cells are paired with neuronal cells, they work together successfully for brain repair and improvement of disease symptoms.
Researchers have long known that understanding brain cell development is vital to understanding and treatment of neuropsychiatric diseases since they hold the key for regeneration. One population of brain cells referred to as the GABAergic interneurons, have the capacity to produce the neurotransmitter GABA, which serve as a signal to guide the interneurons to the right path and are involved in critical functions like memory, language and thoughts. Deficits in GABAergic interneurons in the cerebral cortex have been implicated in neuropsychiatric diseases and are a candidate for cell-based therapy, since it is important to replace what is lost, for successful brain repair.
In more recent years, human cell-based therapies are a treatment that have gained attention, for instance in the case of Parkinson’s disease, as an alternative to prescription drugs or the “shotgun method,” which only treat some symptoms, and can impact many neurotransmitter systems in the brain. But, to date for many other neurological and psychiatric diseases, cell-based therapies have yet to reach clinical trials due to challenges that need to be overcome.
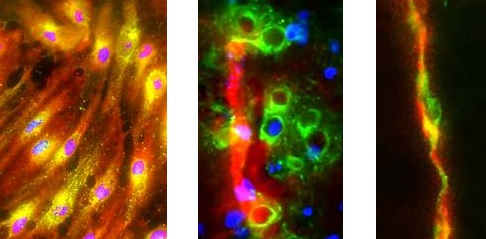
“Cell-based therapy is a transplantation of cells into the brain. For transplantation to be efficient, cells should rapidly travel and integrate with the host brain circuitry in a short time frame. However, on their own, human GABAergic interneurons take several months to migrate after transplantation in preclinical models of disease,” explains Vasudevan. “While studying the mechanics of the cells, we discovered that these GABAergic neuronal cells must be paired with their vascular counterpart, the embryonic forebrain specific endothelial cells for faster, effective therapy.”
“In short,” adds Vasudevan, “we were able to replicate the close neurovascular interactions of the developing forebrain and prove their critical role in guiding the GABAergic interneurons to their final destination in the adult brain.”

Vasudevan says that there is great diversity in vascular populations in the forebrain, and her lab has previously shown how abnormalities in specific brain blood vessels can directly contribute to mental illness. The vascular cells also produce GABA and have GABA guiding components that differ from the interneurons. The team tapped into this knowledge and experience to generate human vascular embryonic forebrain like cells and used them in combination with GABAergic interneurons to reduce abnormal behavioral symptoms in a psychiatric disease model.
“Think of this new cell-based therapy as a story of unity through diversity,” explains Vasudevan, “by combining the unique aspects of two different cell types, we were able to bring out the best in both.”
The study used a GABA pathway component – the GABAA receptor beta 3 subunit (GABRB3) to isolate and generate this new human vascular cell product. This set of the vascular cells is unique to the embryonic forebrain and different from the vascular cells produced in other organs of the body; it is one of the many critical findings from Vasudevan’s work at HMRI that will aide scientists in the longer journey to use cell-based therapies for brain disorders.
“One in four people in the world suffers from a neuropsychiatric disorder,” adds Vasudevan. “That’s 450 million people. Of those, nearly 1 million people commits suicide annually. Today, as a result of the impact of the pandemic, we fear that number could increase substantially. It truly stresses the importance of our work, and the continued need to fund and advance the cell-based therapies forward.”